Image copyright
Family handout
As I wheeled my grandad Martin up the ramp and into a taxi which would take him away to the care home, I repeated the white lie my family had agreed might make this painful scenario slightly easier.
“You’re going to see the physio who will look after your leg and then you’ll be able to get better.”
Thankfully his dementia meant that he couldn’t fully understand what was happening or where he was going. In fact, he seemed to quite enjoy the novelty of being outdoors for the first time in months. But my granny and I were raw with emotion.
Grandad, nonplussed as to why I might be crying, instinctively reached out to stroke a part of my cheek not hidden behind my face mask. Granny blew him a final kiss and the taxi pulled away, leaving me, Granny and my brother-in-law silent in the middle of the street, awash with guilt and relief.
Well into his 80s, my grandad still looked immodestly young and was frequently challenged for his pensioner ID when boarding a bus. During retirement he spent many years volunteering at an elderly care home, caring for people who were often much younger than him.
But as his 10th decade arrived, so did dementia and things started to fall apart. He’d lose track of his words mid-sentence. Making a cup of tea became a challenge. One time the fire brigade descended after he fed a cracker into the toaster. Family rescue efforts were appreciated by my 92-year-old granny, but in truth they were just stop-gaps – like fixing plasters on a broken leg.
“Ageing isn’t for sissies,” she warned me.
When lockdown began, the situation only worsened. Grandad had no understanding of the virus and the changes and restrictions it brought. In late June, my grandparents quietly celebrated their 70th wedding anniversary. Just three days later, Martin moved into a care home. The decision was agonising, but by that point, unavoidable.
Our family’s situation is not uncommon: more than 300,000 people with dementia are living in care homes across the UK, according to Alzheimer’s Research UK. Covid guidelines, which allow limited visiting, at a distance, are designed to keep this vulnerable community safe. But the flipside is families being kept apart from their loved ones, unable to do anything to counter their decline.
Image copyright
Family handout
Julia Hailes with her mother, Minker: “It felt like I’d lost her”
Julia Hailes, a writer who lives in Dorset, has struggled to remain in meaningful contact with her 90-year-old mother, Minker. Minker’s worsening dementia meant her move to a care home was, at first, a lifeline for her family. But the pandemic has changed everything.
“Before lockdown I would visit mum and she still knew who I was. I’d go and read her poems, we’d sit and listen to music,” says Julia. “Now everyone’s being kept in their rooms. It’s vital for people with dementia to have structure in their day, so that isolation is in some ways worse than death.”
Video calls often do little for those with dementia. The notion of holding a “moving picture” of a loved one, as they talk, sounds promising. But it can be a hollow, even disturbing experience.
“Mum’s care home introduced FaceTime calls, which I did a few times,” says Julia. “But it was horrendous. What good is that when someone is in such a confused state? Part of how I connect with her is holding her hand and giving her a kiss. Weeks later I was eventually allowed to visit Mum in the garden. By that point it felt like I’d lost her – she wasn’t even able to speak anymore.”
Image copyright
Family handout
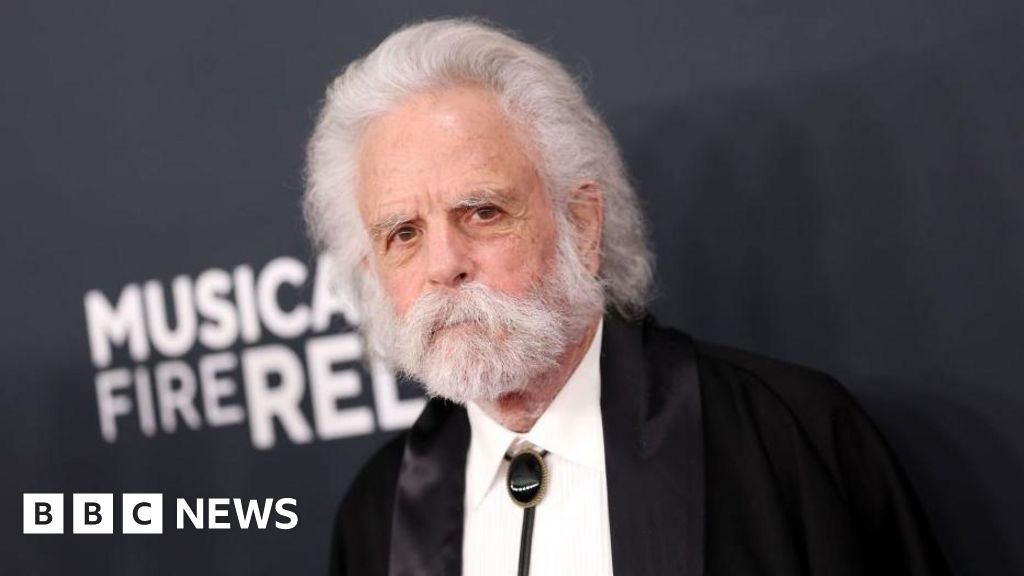
Tom Brada, and his grandad Martin
Dr Hilda Hayo, of the charity Dementia UK, says for people with dementia, technology is no match for human interaction.
“Physical contact is such an essential tool in looking after someone with dementia. If someone is agitated, stroking their hands or putting your arm around them can be really helpful. So, for families, not being able to do that is really damaging.”
This resonates with my own grandad’s experience. Video calls left him more confused than when we’d begun; he could scarcely focus on the screen and struggled to understand where our voices were coming from. The only thing which seemed to cut through was the repetition of a simple message, “I love you, Martin”. To which he could still reflexively respond, “I love you too, Bubala.”
By the time his home was able to permit visitors, his stark decline was clear to my granny. Sunken-cheeked and unable to speak – he was barely recognisable as the man who had left their home just six weeks before.
The dementia of Philippa Thomson’s mother, Marjorie, is so advanced Philippa knew better than to attempt a video call. Before lockdown her in-person visits to the care home would have a restorative effect on her mother.
“We would do relaxing things like colouring in or simple jigsaw puzzles,” she says. “I would sit and hold her hand, or brush her hair. And over two-and-a-half to three days, I would see her coming alive.”
Government guidelines in England only allow for one person to visit each resident indoors; two if it’s outside. But with two older sisters, Philippa has recently been unable to see her mother.
“The carers are amazing, but no matter how good they are, they can’t offer that same intimacy or affection. I do feel a huge amount of guilt and frustration. My mother is 97 years old and it’s not any kind of life that she’s got.”
Image copyright
Mark Harvey
Donna Pierpoint, care home manager
Care homes have borne immense pressures over the past few months. Aware of the burden on both the residents and their families, many made great efforts to maintain a thread of communication. Donna Pierpoint, the manager of a nursing home in Sheffield, described her role in restricting family visits as being “a cross between a prison governor and a headteacher”.
In the meantime she’s focused the home’s efforts on keeping residents as well looked after as possible.
“If someone is being isolated in their room then, you’ve got to take the stimulation to them,” says Ms Pierpoint. “Our staff will go to their rooms and read letters from their family, go through old photographs.”
She sends out a weekly email to keep relatives in the loop and uses social media.
“We post pictures on Twitter, Facebook and Instagram. We celebrated VE-Day on May 8th. We had a wonderful day and posted pictures so our residents’ families could see we were having a good time.”
On 1 August my grandad died at his care home. The majority of his 92 years were happy ones, but his final months were not. The home came to the rescue for my family at our time of need and looked after my grandad wonderfully in gruelling circumstances.
But as relatives, there’s a lingering guilt that we were unable to provide that support ourselves. We did everything we could to let my grandad know how much he was loved. But we cannot shake the sense that the lack of our loving physical presence may have worsened his decline.