Image copyright
Emma Russell
Pregnant women are often now attending hospital appointments on their own. Covid-19 safety measures in hospitals mean loved ones must sit in the car or pace outside. It means some are being given the heartbreaking news of miscarriages on their own. Four women tell their stories of miscarriage during the coronavirus pandemic.
Helen’s story: ‘I won’t try again’
When Helen Bosher, 40, discovered she was pregnant at the end of March, she was anxious – she had lost three babies already, and was under the care of the recurrent miscarriage unit at St Mary’s Hospital, in London. She urgently needed to get hold of some blood test results, but when she rang up she was told her consultant was self-isolating. The unit was closed.
Planned services had been paused and staff re-deployed to urgent and emergency care services. “My whole support network, everyone who was there to help me, just vanished,” says Helen. “They disappeared overnight.”
She frantically rang and emailed her local hospital, her GP and 111, but nobody could help her get hold of the results. “My anxiety went through the roof. I remember crying and crying on the phone, because no-one knew what was going on. It was chaos.”
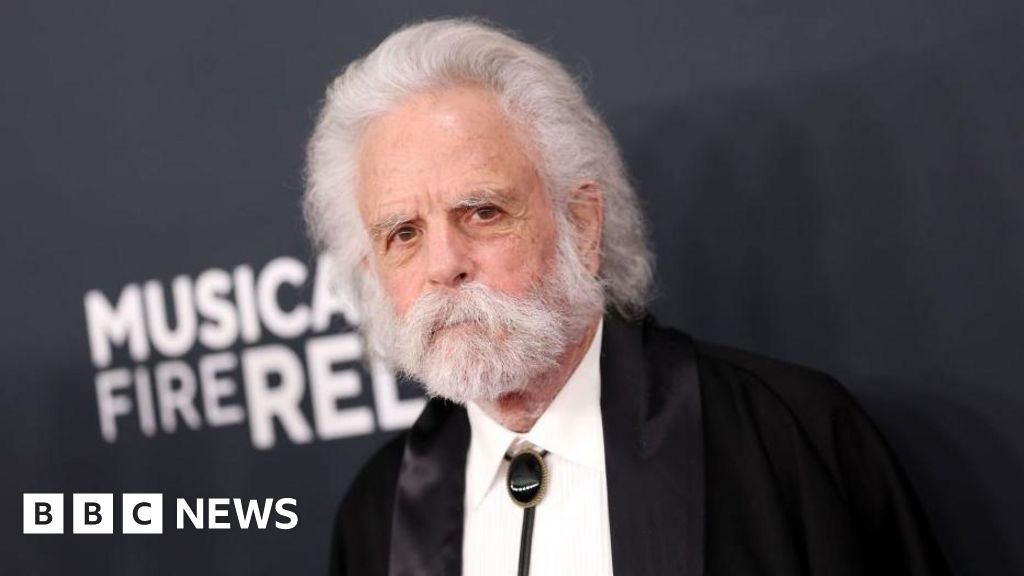
All of Helen Bosher’s support fell away due to the pandemic
Eventually she was booked in for an early scan at Pembury Hospital, in Tunbridge Wells, but because of the new coronavirus restrictions her partner, Dan, was not allowed in with her. It was not good news.
“It was highly distressing to find out my baby had no heartbeat, when my partner had to sit in the car park and wait. I then had to come out and tell him the sad news myself.”
Two weeks later they were back to discuss treatment. Dan stayed in the car while Helen made her way to the early pregnancy unit. She asked a nurse for directions, and when she explained she was miscarrying, the nurse had tears in her eyes. “If only I could put my arm around you,” she told her.
Dan sat in the car, wondering what Helen was going through. It felt strange to see people out shopping and chatting when he couldn’t be with her.
Inside, Helen’s worst fears were being realised. She was given drugs to speed up the miscarriage and the doctors suggested she stay in hospital. But she wasn’t taking in what they were saying – she just wanted to get back to Dan. “I was so overwhelmed and I didn’t have that second set of eyes and ears I needed,” she says.
Five hours later, Helen finally came out. They drove home and waited for the drugs to take effect, but they weren’t prepared for what that involved.
“I ended up having terrible contractions, projectile vomiting, nearly blacking out because of the pain. It was a really terrifying experience,” says Helen.
Dan didn’t know what to do and was desperately searching for advice online. “I was emailing, I messaged people on Instagram,” he says. “Having to Google what’s going to happen rather than speaking to a professional has to be dangerous.”
After four hours the pain and bleeding subsided, but Helen now thinks it was a mistake to go home and that if Dan had been with her she might have chosen to stay in hospital.
The experience was so traumatic they can’t face going through it again. They have decided to adopt instead.
Image copyright
Dan Montague
Dan and Helen have had grief counselling
Maidstone and Tunbridge Wells NHS Trust said that partners are not currently able to attend scan or antenatal appointments, in line with national and regional NHS guidance.
“We understand the concerns this may cause for those who are expecting but we would like to reassure them that the restrictions are in place for everyone’s safety and thank them for their patience and understanding.”
Fatma’s story: ‘It took months’
Just before lockdown, on 16 March, Fatma Reid found out she was pregnant again. The 25-year-old lost a baby the year before, but this time there was no sign anything was wrong. “I had a bump, I was craving Revels, I was definitely 100% pregnant,” she says.
Her six-year-old daughter noticed the bump and kept asking if she was pregnant, and just before the 12-week scan Fatma finally told her she was. But the scan revealed a large sac and no baby. Sometimes called a blighted ovum, or anembryonic pregnancy, this can happen when the foetus dies early in the pregnancy and is reabsorbed, while the sac continues to develop.
“It was very confusing because I’ve never in my life heard of someone having a sac but no baby,” says Fatma. “I was crying loads.”
Image copyright
Fatma Reid
Fatma and her husband Zach
Her husband Zach was called in from the car park to discuss the options. Fatma wanted to have surgery to “get it over with” but operations were being kept to a minimum at the time. She agreed to go home and let nature take its course.
She had to explain to her daughter that she was not going to be a big sister after all – and she waited to miscarry. But nothing happened and three weeks later, she still tested pregnant.
Next, doctors administered tablets to speed up the process. At home, Fatma bled profusely and was in a lot of pain. She hoped that was the end of it, but on 29 June she had another positive pregnancy test.
Back at Salisbury District Hospital a scan showed there was a significant amount of pregnancy tissue left, and surgery was the way forward. Fatma was booked in to have a procedure called manual vacuum aspiration (MVA), under local anaesthetic.
Three days later Fatma was in a lot of pain. “I turned to my husband and said, ‘Oh my God, something’s wrong. This isn’t normal.'” Zach took her to A&E and was initially told to wait outside, until Fatma protested.
- ‘My son was stillborn and now I help other parents’
- Is the risk from Covid-19 higher during pregnancy?
A scan showed abnormal cells, but the doctor was adamant that it couldn’t be pregnancy tissue. “You believe doctors, don’t you?” says Fatma.
Two days later she woke up in agony, bleeding heavily, but she was reluctant to go back to hospital. “You feel, ‘am I overreacting?’ I felt like I was wasting people’s time,” she says.
She rang 111 and they called an ambulance. This time a scan revealed what Fatma suspected – that there was still pregnancy tissue left. She was booked in for emergency surgery on 17 July to make sure nothing was left behind.
Had it not been for Covid, Fatma would have had surgery soon after her 12-week scan. Instead, the process took two months and many hospital visits, all the time trying to hide her distress from her young daughter.
Image copyright
Fatma Reid
Fatma in hospital after her operation – Zach was able to visit her on the ward
A spokesperson for Salisbury District Hospital explained many services had to be altered to protect patients and staff from the virus, and that they are very sorry for any distress caused.
“Throughout the pandemic our staff have sought to do their jobs with care, compassion and commitment especially when helping patients in stressful and upsetting circumstances.”
It is now allowing partners to accompany expectant mothers to their 20-week scan and are keeping all other restrictions under review.
Lauren’s story: ‘I felt I was disappointing him’
Lauren, 33, a teacher from Glasgow, hangs on to the moments of humanity she experienced during an otherwise bleak time. Having first lost a baby last year, she had two further miscarriages during lockdown.
She suspected something was wrong when she started bleeding. A six-week scan in March was inconclusive. But because scans were being kept to a minimum, she was told she couldn’t have another until her 12-week appointment.
“I was pretty sure I was miscarrying again and nobody would confirm it. I was so worried, I was so anxious,” she says.
Image copyright
Emma Russell
Her midwife was able to arrange a scan at nine weeks which confirmed her fears. Lauren begged to have surgery. “I had already had a natural miscarriage at home and was petrified of having another,” she says.
Because of Covid, surgery was not an option. She was booked in for an MVA nine days later, but within days she miscarried at home.
“I had the fright of my life because it sent me into labour,” she says. “Nobody warned me that although my foetus had stopped growing at six weeks, my sac and placenta had continued to grow.”
To ease the pain, she got into a warm bath. Afterwards, she and her husband Michael had to sift through the water to collect the pregnancy tissues. “That was probably one of the most traumatic parts of it.”
They did it because she had been promised the tissues would be sent for genetic testing, in the hope of finding out why she had been miscarrying. But when she took them to hospital the following day, she was told testing had been stopped.
“For us, it was traumatising to find out that after all that, we wouldn’t get any answers,” she says.
Lauren says the worst part of it all was not having Michael with her. She hated having to give him bad news. “I felt like I was disappointing him every time,” she says.
And Michael felt helpless. Instead of getting the facts from a medical professional, he had to piece things together when an emotional Lauren got back in the car. “I’ve got questions that I’ve never been able to ask,” he says. “I’m involved as well. I’ve just been cast out, cast aside.”
Image copyright
Emma Russell
At the start of June, Lauren found out she was pregnant again. When she arrived at the hospital she was overcome by a sense of foreboding.
“I started crying and didn’t want to go out of the car,” she says. “I was worried about going into the building on my own, but my husband wasn’t allowed in.”
Sadly this pregnancy was not viable. Lauren began to miscarry alone at home and made her way to hospital in agony.
“What the midwife did changed everything: she gave me a cuddle,” she says. “She shouldn’t have done that, due to Covid, but it was the right thing to do. It was one of those life-changing moments.”
Lauren now has a supportive consultant and is sharing her experience on Instagram.
Lucy’s story: ‘I had to face this day alone’
For Lucy McLeod, 33, the experience of losing a baby during lockdown felt “a world away” from her previous miscarriage, when her husband Ben was with her.
She was on her own at the 12-week scan when the sonographer could not find a heartbeat.
“I burst into tears, and she put on a pair of gloves to pat me on my knee – I think even that kindness was against protocol,” she says.
Image copyright
Lucy McLeod
Lucy says she couldn’t face going through labour
“I was sent to a different room to talk to a midwife who, after asking me to sanitise my hands, cautiously put a box of tissues between herself and me. She said they would usually offer a hug right now, but she wasn’t allowed to.”
Lucy was offered options that would not require surgery, but she rejected them. “I couldn’t face going through labour to birth a baby that was dead. It felt like a second blow that I would have to give birth to her and clean her up myself in order to bury her,” she says.
It was agreed that she could have surgery, but she had to accept the risk of catching the virus while in hospital. “Even so, I much preferred this option,” she says.
Lucy was swabbed for Covid before being wheeled into theatre. She was still crying when she came round. “The sister in recovery stroked my hair and held my hand tightly. I was so grateful for her soothing me,” she says. “I couldn’t believe that I had to face this day alone.”
Ben and Lucy have named their baby Chloe. They will collect her body this week. But Lucy is worried about the effect Covid measures will have had on the mental health of people who have lost a baby.
Image copyright
Lucy McLeod
Ben and Lucy named their daughter Chloe
“Miscarriages are devastating,” says Birte Harlev-Lam from the Royal College of Midwives. “We know that this pandemic has made the experience even more difficult due to restrictions on having partners at scans and other appointments.”
The miscarriage charity Tommy’s saw a huge spike in helpline queries during the pandemic and is urging women to seek medical help if they have symptoms such as changes in their baby’s movements, severe pain or heavy bleeding.
According to Royal College of Obstetricians and Gynaecologists guidance, scans should still be offered if someone is worried about retained pregnancy tissue, if they’re bleeding heavily, or if they’re in pain, and women should then be monitored for signs of infection.
Consultant gynaecologist Prof Tom Bourne, speaking for the RCOG, says a study is being done on the impact of the pandemic on the care of women with complications in early pregnancy, including miscarriage, and that those experiences will inform future guidance.