Catherine Burns,Health correspondent ,
Vicki Loader,Health producerand
Harriet Agerholm
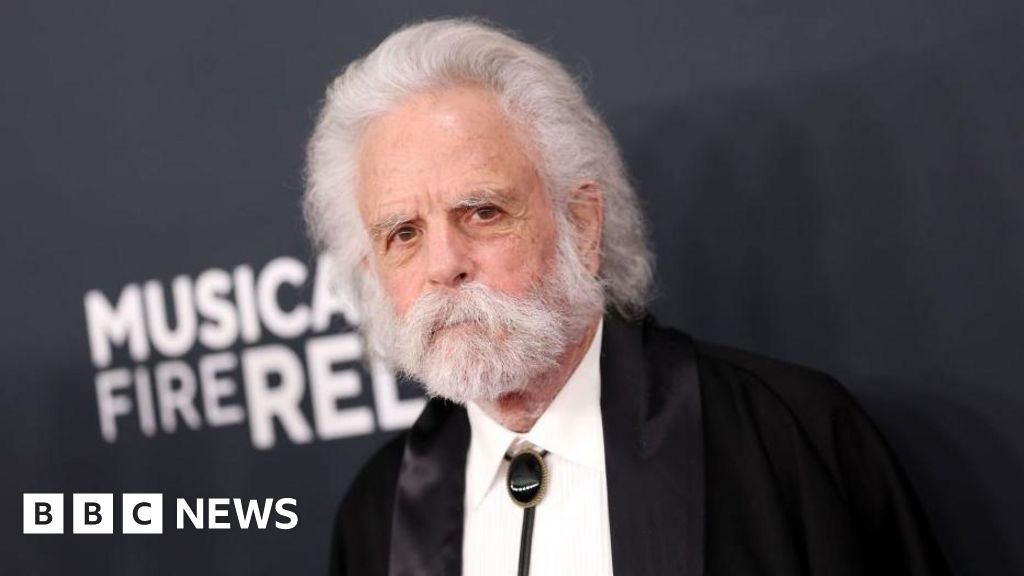
 Getty Images
Getty ImagesHundreds of GPs across England have told the BBC they think mental health problems are being over-diagnosed.
One commonly-held view by family doctors, our research suggests, is that society tends to over-medicalise normal life stresses. But they’re also concerned about how hard it is to get help for patients with mental health conditions.
Earlier this week, the Health Secretary ordered an independent review into the reasons for a rising demand for mental health, ADHD and autism services in England, and where the gaps in support are.
BBC News sent a questionnaire to more than 5,000 GPs in England asking about their experiences helping patients with mental health concerns. Their responses give an insight into how challenging this issue is for many family doctors.
Of the 752 GPs who took part in our research, 442 said they believed that over-diagnosis is a concern. More said mental health problems were over-diagnosed by a little than over-diagnosed by a lot.
Eighty-one GPs who responded felt that mental health problems were under-diagnosed.
Over-diagnosis of mental health issues was far from their only concern. Many GPs also told us they were worried about a lack of help for patients.
For our questionnaire, GPs answered several questions and were invited to leave anonymous comments.
One of the most common themes to emerge can be summed up in this remark from a GP: “Life being stressful is not an illness.”
Another commented: “As a society we seem to have forgotten that life can be tough – a broken heart or grief is painful and normal, and we have to learn to cope.”
Yet another argued that giving people labels such as anxiety or depression “over-medicalises life and emotional difficulties”, and that this was taking resources away from people with severe needs.
A small number of GPs were strongly critical of some patients. One described them as “dishonest, narcissistic… gaming a system free at point of use.”
Overall, one in five adults in England report having a common mental health condition, like anxiety or depression, according to a survey published by NHS England. Rates are even higher in young people. For 16-24 year olds, it’s one-in-four.
The GPs who took part in our research identified 19-34 year olds as the age group who needed the most support with mental health issues.
One commented that young adults “seem to be less resilient since Covid”, suggesting they’re more concerned with getting a diagnosis than finding coping strategies.
But other GPs said the real issue was under-diagnosis.
“People need to be accepted, helped and encouraged to live life,” one said, while another said services were very reluctant “to fully assess and diagnose” patients.
There are almost 40,000 fully-qualified GPs in England and we cannot know if the group who took part in our research is representative of all family doctors.
We asked GPs who had been in the job for at least five years how the amount of time they spend working on mental health has changed. Almost all said it has increased.
The three main reasons they gave for this were:
- having to support patients who can’t get good quality mental health help elsewhere
- practical issues like housing, employment or finances impacting patients’ mental health
- patients thinking they have a mental health issue, when they’re dealing with normal challenges in life
Earlier this year, the health secretary Wes Streeting told the BBC’s Laura Kuenssberg that mental health conditions were being over-diagnosed and too many people were being “written off”. He now says his comments were “divisive” and that “he failed to capture the complexity of this problem.”
And it is, undoubtedly, a problem.
It is thought that 2.5 million people in England have ADHD – including those without a diagnosis. Some NHS services for ADHD have closed their doors to new patients because they are struggling to cope with the demand.
Patients have told the BBC about how hard they find it to get proper care and support.
All in all, there’s a consensus that the NHS is not meeting rising demand in this area.
A clear majority of GPs who took part in our research, 508 of 752, said there was rarely or never enough good quality mental health help available for adults in their area.
Even more, some 640 GPs, told us they were worried about getting young patients the help they needed.
One GP called mental health support “a national tragedy”. Another said: “A child literally needs to be holding a knife to be taken seriously and the second that knife is put down, services disengage.”
We also asked GPs if they ever prescribe medication because they worry patients will not get other help, such as talking therapies, quickly enough.
The most common answer – from 447 GPs – is that they do this “routinely”.
“I find myself regularly reaching for antidepressants, which I know may only help short term and won’t help prevent recurrence,” one GP commented.
Professor Victoria Tzortziou Brown, chair of the Royal College of GPs, said there’s a “difficult balance” for family doctors to strike when patients expect a diagnosis for mental health problems, but don’t meet the criteria.
“We must be careful, as a society, not to medicalise the full range of normal feelings and behaviours and ensure GPs are not pressured into making diagnoses that conflict with their clinical judgement,” she said.
“But equally we must avoid dismissing genuine mental health concerns as ‘over-diagnosis’ which risks discouraging people from seeking help.”
The independent review into demand for mental health services has promised to listen to all the evidence and come up with “genuinely useful” recommendations.
Additional reporting by Phil Leake.